Kits distributed across province to help reduce opioid deaths
MANITOULIN—Five pharmacies on Manitoulin Island are among the over 200 cities and towns in Ontario where access has been expanded by the province of Ontario to a life-saving drug that can temporarily reverse an opioid overdose. The drug is being provided free of charge.
Dr. Eric Hoskins, Minister of Health and Long-Term Care, was joined on April 11 by Marie-France Lalonde, Minister of Community Safety and Correctional Services, to raise awareness about Ontario’s naloxone program and to encourage more people who are at risk of an opioid overdose, as well as their friends and families, to pick up a free kit.
As of the end of March 2017, more than 28,000 naloxone kits had been dispensed free of charge at over 1,000 pharmacies, and at 40 public health units and community-based organizations that run needle exchange and hepatitis C programs. In addition, more than 500 naloxone kits have also been distributed at 10 provincial correctional facilities to at-risk inmates at the time of their release. By the end of spring 2017, all 26 provincial correctional facilities will be able to distribute naloxone kits.
On Manitoulin Island, the naloxone kits are to be available at both the Central Pharmacy and Robertson’s IDA in Gore Bay, the Little Current Guardian Pharmacy and the Edgewater Pharmacy in Little Current and the Mindemoya Medical Pharmacy.
“I’d like to thank the many health care workers in our communities who are helping to save lives by getting naloxone kits to the people who need them. Ontario’s naloxone programs are an integral part of our comprehensive strategy to prevent opioid overdoses by putting people and patients first,” said Dr. Hoskins.
Ms. Lalonde said in part, “the opioid crisis is a growing threat. Vulnerable people need access to this life-saving drug, and providing inmates with naloxone kits upon discharge from our correctional facilities will save lives.”
Expanding access to opioid overdose medication is part of Ontario’s Strategy to Prevent Opioid Addiction and Overdose. As part of this strategy, Ontario has also delisted high-strength opioids from the Ontario Drug Benefit formulary to help prevent addiction and support appropriate prescribing; launched a comprehensive website about Ontario’s naloxone kit programs, which includes information on how to use naloxone kits, how to prevent an opioid overdose and a searchable list of where kits are available across the province; and placed stricter controls on the prescribing and dispensing of fentanyl patches. Patients are now required to return used fentanyl patches to their pharmacy before more patches can be dispensed.
Opioids are drugs that are intended to treat pain. Some commonly used opioids include fentanyl, morphine, heroin, methadone and oxycodone.
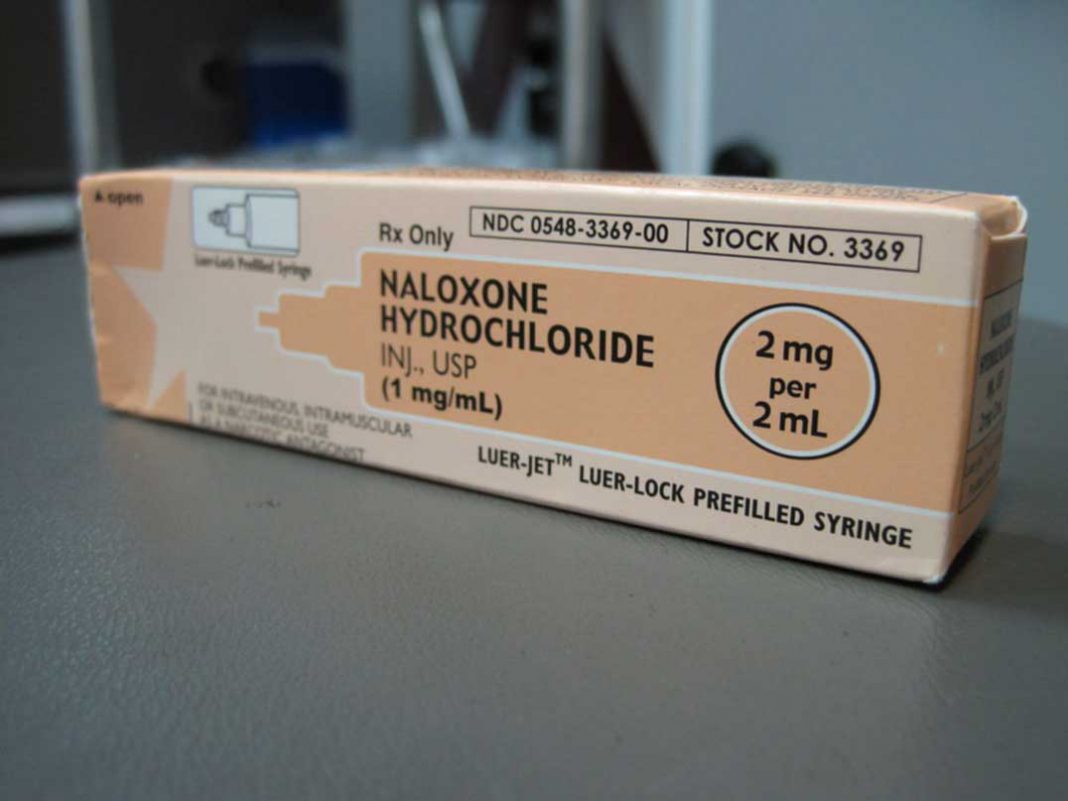
When someone overdoses after taking an opioid, their breathing slows or stops. Naloxone is a medication that can temporarily allow the person to breathe normally and regain consciousness, providing precious time to seek emergency medical attention to treat the overdose.
Anyone who gets a naloxone kit through one of Ontario’s programs will also receive training on how to recognize an opioid overdose and how to use the naloxone kit.
Dr. David Williams, the Chief Medical Officer of Health Provincial Overdose Coordinator said, “approximately one in every 170 deaths in Ontario is opioid-related. If we are going to reverse this troubling trend, the entire health care system must continue to work together. Distributing naloxone kits to those at risk of an overdose and their friends and families is an important step in the right direction.”