Out of the Shadows
An in-depth look at Manitoulin’s opioid crisis
The Long Read
Share on facebook
Share on twitter
Share on reddit
Share on email
Share on print
EDITOR’S NOTE: ‘Out of the Shadows’ first appeared as a special supplement to the June 23, 2021 edition of The Manitoulin Expositor. Statistics are likely to have changed in the months that followed. The Expositor wishes to give a special thanks to the late Tony Jocko for his help with the project, and all others who contributed and shared their stories. Please know that you are not alone.
If you or someone you know is struggling with addiction, supports are available.
Introduction
The COVID-19 pandemic has formed the global public health crisis of a generation but the Manitoulin and Sudbury areas have avoided its worst effects. At the same time, as the public celebrates flattening infection curves and begins to dream of returning to “normal,” a second, older emergency has only gotten worse. This crisis, however, remains out of sight and mind for many people.
In 2020, 2,426 Ontarians died from opioid-related causes, an increase of almost 60 percent over 2019 figures. Some months saw death rates as high as eight per day in the province.
Opioid-related deaths in Ontario rose 75 percent during the first three months of COVID-19 restrictions, but those rates have not slowed even as the pandemic begins to ease. On May 12, 2021, staff at one Toronto overdose prevention site reversed 14 overdoses in a single day.
Despite perceptions of addiction as being a largely urban problem, statistics show Northeastern Ontario has had the highest rates of opioid-related deaths since the start of the pandemic.
Manitoulin Island is not exempt from that trend, where reported deaths have more than tripled during the pandemic compared to 2018 and 2019 figures. Rural areas create unique challenges to accessing care and advocates, community leaders and drug users alike are desperately seeking innovative solutions and government support.
As COVID-19 cases drop and a public health success emerges, another public health tragedy continues to worsen with no signs of improvement.
About the writer
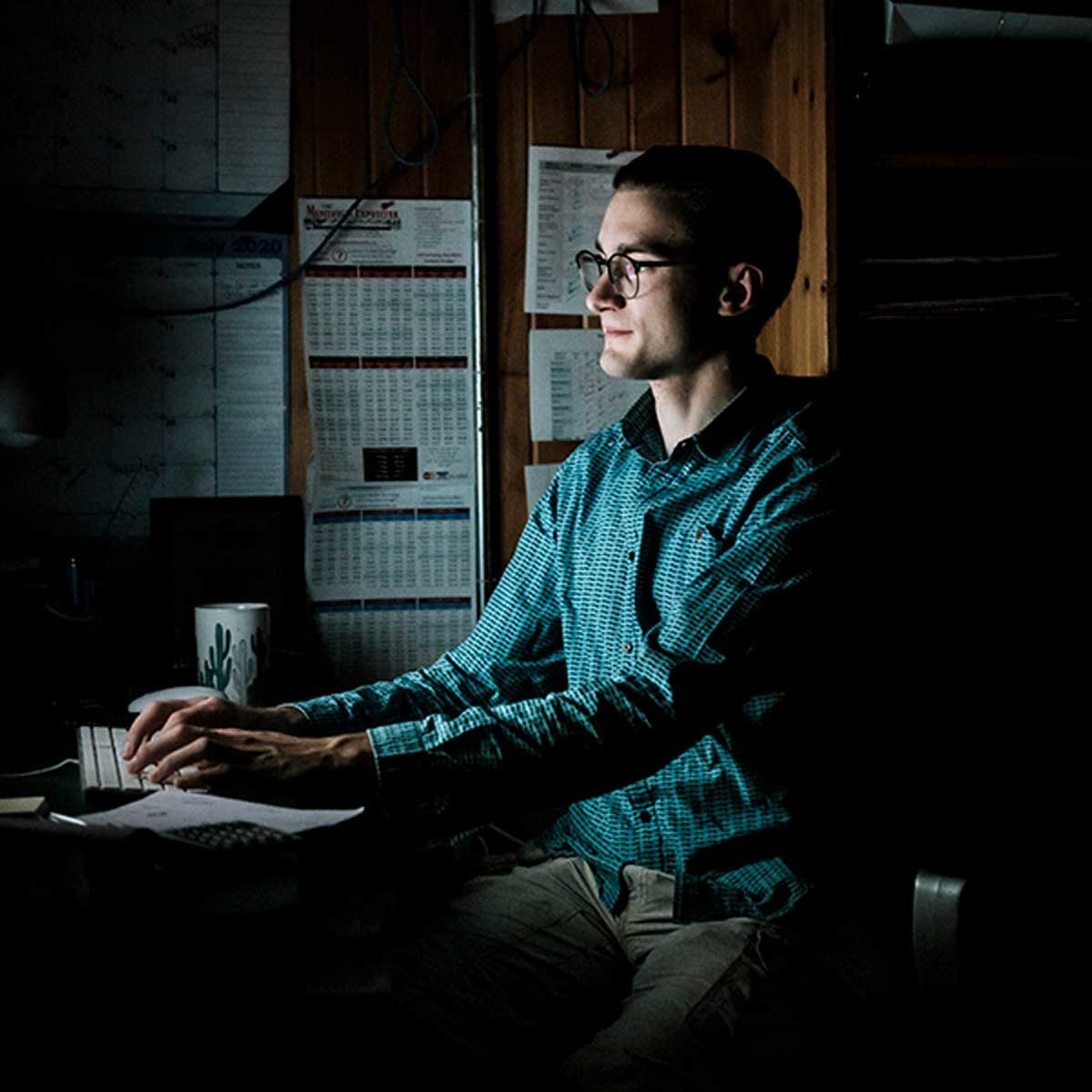
Warren Schlote is a multimedia journalist who has worked with The Manitoulin Expositor for three years. His reporting has covered topics including historic sexual abuse by priests serving a First Nation, environmental issues impacting Manitoulin, the hidden problem of male-victim family violence and developing police situations.
He began work on what became Out Of The Shadows in late 2020, after hearing community members talk about a sharp rise in overdoses on Manitoulin Island. He was not well-versed in the scope of the crisis and decided to turn his own research process into a long-form educational piece to help others understand the issue as well.
Warren spends most of his working time as a reporter, editor and associate producer at CBC Sudbury.
About the photographer

Giovanni Capriotti is an award-winning photographer who specializes in long-form in-depth documentary explorations that examine how time and inevitability of compromise shape individuals, communities, history, culture, and human condition. He is the 2017 winner of the prestigious World Press Photo award and has other international accolades to his name. Giovanni has also taken top honours in several categories from the Ontario Community Newspapers Association Better Newspapers Competition on behalf of The Manitoulin Expositor.
Giovanni was inspired to shoot specially for this project after reading the print version of “Out of the Shadows.’ You can see more of his work at: www.giovannicapriotti.com
Chapter one
Dr. Lionel Marks de Chabris is a pain management and addictions specialist.
In his 32 years working on Manitoulin Island, physician and coroner Dr. Dieter Poenn has seen the worsening crisis firsthand.
“Drugs have always been in the background, but it’s never been in the foreground as much as it is now,” he says.
According to coroner records, seven people died on Manitoulin Island last year from opioid-related causes. In 2018 and 2019, the annual figure was just two deaths.
Paramedics and coroners say they fear the real death statistics may be even higher, including cases where opioids had contributed but were not necessarily the main cause.
In the Sudbury and Manitoulin areas over the past year, there were nearly four times more drug-related deaths than those from COVID-19.
That number of “unnecessary deaths” has been a shock for Detective Sergeant Todd Fox of Wikwemikong Tribal Police Service (WTPS). He helps lead that force’s work against the criminals entering Wiikwemkoong to sell narcotics and profit off its vulnerable citizens.
“That should be a big red flag for societies and communities to come together to do the best they can … to prevent overdose deaths,” he says.
Manitoulin-Sudbury District Services Board (DSB) Paramedic Services is one of the agencies most involved in the crisis on Manitoulin. Its members are often the only ones that can prevent overdoses from turning fatal.
But understanding the full scope of the Island’s opioid problem is complicated, even for paramedics. Paul Myre, chief of paramedic services with Manitoulin-Sudbury DSB, says there are often multiple medical factors involved in health emergencies.
“That should be a big red flag for societies and communities to come together to do the best they can … to prevent overdose deaths,”
Joe Naokwegijig, an officer with the UCCM Anishnaabe Police Service, has seen first-hand the devastating effects of the crisis on the communities he serves.
This means his team members have to log ‘suspected opioid overdoses’ based on the patient’s condition and what clues may remain at the scene.
“(Our statistics are) not the total picture, as there are several sudden cardiac arrests that cannot be 100 percent attributed to an overdose as the cause due to a number of variables, but would be considered highly suspicious,” Mr. Myre says. “Sadly, my assumption would be that the picture is much more grim than the one painted below with that specific data set,” he says. “The (younger) age of some of the sudden cardiac arrest patients leads me to suspect something other than a cardiac event, but … we are not privy to post-mortem results.”
The data he shares with The Expositor cover part of 2018 through to the beginning of May 2021. In 2018, paramedics responded to at least five calls for suspected opioid overdoses on Manitoulin Island. By 2019, that number was 20. In 2020, it grew two-and-a- half times to 48.
Island paramedics have administered naloxone, the overdose reversal drug, 13 times since 2018. Mr. Myre says medics may choose to not use naloxone if they can support a patient without it.
In the first four months of 2021, paramedics had already attended to 19 suspected opioid overdoses in the District of Manitoulin.
An OPP tweet from February states officers have saved 210 lives since they began carrying naloxone in 2017, but the frequency of naloxone use grew 38 percent between 2019 and 2020.
OPP officers have saved 210 lives since they began carrying naloxone in 2017, but the frequency of naloxone use grew 38 percent between 2019 and 2020.
Manitoulin opioid deaths
Deaths involving opioids per year for
Manitoulin Island
Island-based doctors are noticing the uptick in their practices, too.
Dr. Shelagh McRae, a Gore Bay-based doctor who also serves as coroner for the West End, says she has seen more opioid-related deaths and substance use disorder among her patients over the past few years.
“There’s several factors, but I think two main ones are the fact that there are very potent opioids available and people often don’t realize what they’re taking until it’s too late. The second is the pandemic has shut down a lot of the social and work outlets people might have instead of turning to drugs,” she says.
The drug crisis does not discriminate based on demographics. Although Dr. McRae says she can’t disclose the detailed opioid-related death statistics from her coroner work, she says the problem absolutely exists in both First Nations and non-Indigenous populations.
It’s devastating drug users and dividing families, such as “Jean” from Little Current, who buried her 36-year-old son this past fall after a fatal overdose. The Expositor has withheld her real name upon request due to family tensions.
“These drugs are ruining a whole generation of kids,” she says. “(Drugs get) here to the Island just as fast as anywhere. I look at the obituaries and how many times it says young kids in their 20s and 30s ‘died suddenly’ over the last year. It was quite a few people (my son) knew.”
Every Manitoulin resident can feel the impacts of the opioid crisis, even if it has not reached their family. This is heightened because of the small size of Island communities, in which word travels fast about who has died and why, Det. Sgt. Fox says.
“The community is in mourning because, I think, the community collectively knows this is an unnecessary death and should have been preventable and avoidable,” he says.
Anishinabek Nation federal health policy analyst Tony Jocko agrees.
“Communities are really hurting because they’re losing a lot of young people, which they feel is (unnecessary), and they’re really struggling to understand why,” he says
The community is in mourning because, I think, the community collectively knows this is an unnecessary death and should have been preventable and avoidable
Opioid overdose calls
Total opioid overdose calls on
Manitoulin Island
(Note – 2021 is Jan to May 6)
Although the opioid crisis affects people on Manitoulin Island as it does in urban settings, communities struggle to get information about the impacts it has on their people.
Public health staff and first responders are often reluctant to share detailed information about suspected overdoses with local governments because of legitimate privacy concerns. First Nation police forces are one access point to this information because if they get called to a suspected overdose scene alongside paramedics, they can report that to their constituent band councils.
First Nation police services on Manitoulin Island also have officers who can issue press releases on their drug-related operations. The Manitoulin detachment of the Ontario Provincial Police (OPP) does not currently have anyone in such a role, which helps the public stay informed on these threats.
Municipalities rarely have direct options because their health, social services and law enforcement agencies operate in separate silos. First Nations, in contrast, tend to be more vertically integrated as they have to run many of their social services on their own.
Take M’Chigeeng as an example: the First Nation has its own health centre and M’Nendamowin, a mental health and addictions program; a First Nation police service headquartered within its territory and its own elementary school.
In a municipality like the Northeast Town, its local family health team reports to the province rather than the local government. The health team offers addictions services through Northwood Recovery, an outside provider.
The Northeast Town receives policing from the Manitoulin OPP detachment, which also includes several thousand square kilometres on the North Shore. Education goes through the Rainbow District School Board and all other services such as social housing and Ontario Works funnel through the Manitoulin- Sudbury DSB, which serves a 45,000- square-kilometre area.
Each service provider has its own administration and policies about information sharing. All ultimately report to the province. Besides periodic summary reports of their partners’ activities, rural municipalities tend to have few insights into the health of their citizens.
This disparity has the twofold effect of making the drug crisis falsely seem like a First Nations issue to solve, despite its presence across all of Manitoulin. It also keeps municipal leaders farther away from the problem and hinders their ability to fully understand and make meaningful progress on the file.
That’s frustrating for Northeastern Manitoulin and the Islands (Northeast Town) Mayor Al MacNevin, who says his council desperately wishes to be part of the solutions. He says the only information he gets on overdoses in his municipality are when a community member tells the town office or there’s media coverage.
“We don’t really have a handle on the issue at all,” Mayor MacNevin says. “We tried to find a way around that so we could educate ourselves on how serious it is.”
He explains that the township has previously tried to work with the DSB to get more information on overdose deaths, but the only data they could access was district-wide. Having more granular data would help to reveal the realities in each community.
“In the long term, it’s going to help out everybody to … know that this is not some imaginary tale, this is happening in their community,” Mayor MacNevin says.
“We don’t really have a handle on the issue at all, we tried to find a way around that so we could educate ourselves on how serious it is.
Aaron Case was the second person in Canada to receive the life-changing probuphine implant, considered among the top opioid maintenance treatments.
Although First Nations’ structures can help them better understand the drug crisis in their communities, it also means their governments face an overwhelming number of responsibilities.
Keeping a First Nation running is already a full-time job, but as the opioid crisis worsens, chiefs frequently get asked to help community members at all hours, are helping to organize funerals and to connect people with the supports if other providers aren’t available to do so.
First Nation leaders find themselves increasingly on the front lines of the crisis, taking on far more responsibilities than a chief’s job description would include.
The present lack of information sharing does not have to be the default. Larger municipalities generally have a much better understanding of drug crises among their citizens than rural communities.
Sudbury, for instance, receives regular updates on the state of the opioid overdose crisis through its Community Drug Strategy, a partnership with Public Health Sudbury and Districts (PHSD), police and the city. Those data show a concerning trend among its population.
In 2019, paramedics responded to 468 suspected overdoses in the City of Greater Sudbury; that number rose to 683 in 2020, a 46 percent growth year-over-year.
The trends appear to be worsening into 2021.
In the first three months of this year, Greater Sudbury Paramedic Services responded to 216 suspected overdoses, 55 percent more than the first three months of 2020.
PHSD hosts Community Drug Strategy’s data on its website, which offers a public snapshot of the addictions and overdose crisis in that city. Such resources do not exist for Manitoulin Island.
The Island’s local response group is Manitoulin Drug Strategy, which does not have a web presence of any kind. Any data it might have on the state of addictions and overdoses on Manitoulin Island are not accessible to help the public understand the situation at home.
The Expositor has been seeking information from Manitoulin Drug Strategy co-leads Katie Gilchrist and Mark Forsythe about the work the group is doing to combat the opioid crisis, but this newspaper has struggled to get information (or responses to enquiries) from its leaders.
Other health officials with ties to Manitoulin Drug Strategy have said several people involved with this effort, including a project lead, are presently redeployed for COVID- 19 vaccination efforts, which may explain the difficulty in making contact.
Mayor MacNevin says regular updates on the health of the community, particularly on public health crises such as the opioid epidemic, may get more municipal leaders engaged in Island-wide efforts to address the problem.
Fentanyl
Fentanyl is a synthetic opioid that’s roughly 50 to 100 X
more potent than morphine (a natural opiate). Morphine becomes lethal at a dose of 2,000 micrograms but fentanyl can kill at just 700 micrograms.
Even stronger is its analog, carfentanil, an elephant tranquilizer, which is about 100 times stronger than fentanyl or 10,000 times stronger than morphine.
In the first three months of this year, Greater Sudbury Paramedic Services responded to 216 suspected overdoses, 55 percent more than the first three months of 2020
As the opioid crisis evolves, it brings new impacts to Island communities, including increasing levels of violence and intimidation on the part of drug traffickers.
“This year, we’ve had two separate events that involved seizing firearms in relation to circumstances surrounding the drug subculture,” says Det. Sgt. Fox, describing the trends in Wiikwemkoong. “Firearms are starting to become more common.”
Dealers often equip themselves with weapons for personal protection and to collect debts, but drug users may also arm themselves in response, Det. Sgt. Fox says. It’s a sort of arms race between the two sides and crime statistics show growth in violent incidents in recent years.
Among the higher profile incidents as of late, drugs have been a factor in the 2019 M’Chigeeng shooting and subsequent takedown at the swing bridge, the double-fatal Gore Bay shooting from last November and, most recently, the emergency alert from early May when an armed-and-dangerous suspected drug dealer ran from police.
Island leaders and advocates are calling for better solutions for the opioid crisis’ contributing causes of addictions and mental illness.
In the meantime, the crisis will continue to ruin lives of all ages, even children. Anecdotally, children’s aid workers in the Sudbury- Manitoulin area tell The Expositor that they frequently encounter drugs in situations when care societies have to intervene.
Sudbury-Manitoulin Children’s Aid Society executive director Elaina Groves agrees that drugs are a major issue in the families connected to her organization, but she cannot provide any statistics about the issue. Just as municipalities struggle to understand how badly opioids impact their people, the provincial children’s aid case management system is not set up to capture the factors in care decisions.
“Our knowledge is not data-based, it’s anecdotal, and we are concerned about that,” says Ms. Groves, who explains that in order to create statistics about the prevalence of drugs in children’s aid cases, workers would have to go through files manually.
She says there have been past discussions about improving the system, but these did not lead to changes. The Expositor’s inquiry, she says, has prompted her agency to restart discussions at the provincial level about improving the tracking and analysis of these causal factors.
“This (data) would bring public awareness and can influence our governments,” she says. “How can we truly understand the degree or the nature of the problem in order to address it and advocate for it, unless we can collect the data?”
This year, we’ve had two separate events that involved seizing firearms in relation to circumstances surrounding the drug subculture.
Chapter two
A man pays his respects at the memorial to those lost to the opioid crisis on M’Chigeeng First Nation.
To better understand the overdose crisis, it helps to understand opioids. Opioids (a term that includes natural, synthetic and semisynthetic drugs; opiates strictly refers to naturally occurring opioids) are drugs that act as painkillers. Wellknown opioids include codeine (Tylenol 2, 3 and 4), hydromorphone (Dilaudid), morphine, oxycodone (Percocet, related to its synthetic counterpart OxyContin) and fentanyl, among many others.
Opioids are depressants, a category of drugs that includes alcohol, which means they block neurotransmitters. Opioid molecules attach to receptors in the body’s cells and suppress sensations of pain. They can also produce a high.
These drugs kill because they disrupt the functions of the central nervous system, including one’s breathing and heart. The higher the dose of opioids, the stronger the effect on the unconscious part of the brain that controls breathing.
“Once you suppress it to the point where it stops working, you stop breathing and you die,” says Dr. Lionel Marks de Chabris, a pain management and addictions specialist who services some Island patients through his Espanola clinic.
Dr. Lionel, as his patients call him, provides consultation and educational services about drugs and has spoken at Island conferences in years past.
He says substance users are split into two parts: recreational users who can stop at any time, and those who acquire a use disorder, which is a mental illness. This is a life-threatening condition that makes the brain believe opioids are the most important thing it needs to function.
“We know that people will give up everything— marriages, children, cars, homes, jobs, everything—because the drug is more salient than anything else. These people desperately need help,” Dr. Lionel says.
Opioids also have a multiplying effect. The body develops tolerance to their presence and the user will require larger doses to get the same painrelief effects, which can lead to use disorders.
The US Food and Drug Administration states that if a person has been taking a daily dose of 60 milligrams of morphine or equivalent (two 12-hour Oxy- Contins, for example) for one week or longer, they begin to develop opioid tolerance.
At the state of dependence, when a dose wears off, a user will enter withdrawal. This often leads to the user trying to find more of the drug at all costs, even if it requires behaviour they know is morally wrong, such as violence or theft.
Cutting off the supply at this point is not enough to make a user’s problem go away.
The substances behind overdose crises have evolved over the years, Dr. Lionel says, from OxyContin in the mid-2000s to heroin, then fentanyl. Fentanyl and its even-morepotent analogues remain the biggest current threats in the opioid overdose crisis.
We know that people will give up everything— marriages, children, cars, homes, jobs, everything—because the drug is more salient than anything else. These people desperately need help
What‘s being found in street drugs?
Statistics from Toronto’s drug check stations, which offer free, anonymous analysis to reveal what’s in users’ drugs, show that opioids were the most common type of drugs to also contain other substances.
The Toronto figures, says Inspector Slaughter, are important in the North because Manitoulin’s illicit drugs tend to originate there.
In 2020, Toronto’s Centre on Drug Policy Evaluation found 95 percent of drugs labelled as fentanyl had other substances within them, and every single sample of heroin had at least one other substance mixed in.
Three-quarters of the fentanyl that led to an overdose also contained benzodiazepines (‘benzos’).
Non-opioids are liable to be laced, too. Only 55 percent of cocaine samples contained no other substances and the frequency of cocaine additives doubled in 2020 alone.
There are no drug toxicity stats specific to Manitoulin Island, though Sudbury Action Centre for Youth launched a drug check service in 2019.
Drug check services are not the ultimate tool to prevent overdoses. Checking a few pills cannot guarantee that there won’t be ‘hot spots’ in other parts of the batch.
Fentanyl is a synthetic opioid that’s roughly June 23, 50 to 100 times more potent than morphine (a natural opiate). Morphine becomes lethal at a dose of 2,000 micrograms but fentanyl can kill at just 700 micrograms.
Even stronger is its analog, carfentanil, an elephant tranquilizer, which is about 100 times stronger than fentanyl or 10,000 times stronger than morphine. Over the past year, Dr. Lionel has seen street drug warnings after drug check stations found opioids not approved for use in humans (notably etizolam, a benzodiazepine), drugs previously banned because they caused kidney disease and cancer, as well as large animal tranquilizers associated with higher hepatitis rates in humans.
Economics help to drive super-strength opioids into street drug supplies. Fentanyl is relatively cheap to produce and illegal drug makers can save on costs by mixing fentanyl with other substances, offering high potency with fewer materials.
While many drug users seek it out intentionally, fentanyl often appears with no indication to the end user or may be accidentally introduced into a batch. “That’s the scary thing about these medications. You may only try them once, not knowing what you’re actually taking, and you may never wake up,” says Mr. Jocko, the Anishinabek Nation analyst.
“Many times, drug users … think they’re purchasing one thing and it ends up containing something that can be fatal,” says Inspector Cori Slaughter, director of operations at UCCM Anishnaabe Police Service, which offers policing to United Chiefs and Councils of Mnidoo Mnising communities in the District of Manitoulin.
Medical-grade opioids are far less likely than street drugs to cause an accidental overdose, unless the user consumes them in an unintended way. However, those safer drugs are increasingly difficult to access.
The Northern Opioid Crisis
+60%
2019 to 2020
Public Health Ontario says more than 2,400 people died in the province in 2020, up 60 percent from the 1,517 deaths reported in 2019.
Fentanyl was involved in 87 percent of opioid deaths during the pandemic up from about 75 percent before the virus. The highest rates of opioid deaths during the pandemic were all in Northeastern Ontario, including the Public Health Sudbury and Districts (PHSD) area. Further Public Health Ontario data show PHSD’s rates of opioid deaths were three times higher than the whole province before the declaration of the pandemic on March 11, 2020. The gap has only since widened.

The Sudbury-Manitoulin area saw 11 opioids deaths per 100,000 citizens in the 15 weeks before the pandemic declaration, which rose to 14 per 100,000 for the 15 weeks after that date.
Opioid prescriptions have dropped dramatically from their heyday in the 2000s, before people began to realize the dangers of substances like OxyContin. Some advocates argue the current prescription levels are too low, but physicians tend to be apprehensive about prescribing them after learning how harmful they can be.
These measures, however have come too late. A substantial number of opioid use disorder patients started on prescription drugs, which were so freely in abundance in the 1990s and 2000s. Manitoulin was ahead of many areas in reducing opioid prescriptions, recall Island health providers.
“We hardly prescribe those drugs here anymore because of all the abuse problems we see coming to the surface,” says Dr. Poenn, the physician and coroner.
Little Current pharmacist Chris Gauthier says he has noticed a drop in prescriptions for opioids, namely oxycodone, and for good reason.
“(Oxycodone) in particular is extremely addictive and habit-forming and very difficult to discontinue once a patient becomes physically and psychologically dependant on the chemical,” he says.
Health Canada has also dropped recommended opioid usage amounts for non-cancer chronic pain patients.
Ontario Drug Policy Research Network tracks the number of opioid drug prescriptions that pharmacies fill across the province, with a data set that begins in July 2012.
The data peaks in October 2013 when Ontario pharmacies distributed about 872.5 million doses. It has since gradually dropped to near half of that amount, resting around 471 million doses dispensed each month in late 2020. The downward trend is flattening off.
When narrowing the statistics to the PHSD boundaries, prescriptions peaked at roughly 18.5 million in October 2012. Its numbers also dropped nearly in half and this health district now averages around 9.5 million doses per month. When averaged among the whole population of the PHSD area, per 2016 figures, the equivalent would be every person receiving 48 opioid doses per month. This remains well above the provincial average of 32 monthly doses per capita.
The drop may help new patients from ever getting on opioids, but the same decline could help to fuel the overdose crisis as dependent drug users turn to unpredictable, illicit supply chains.
When Island prescribers began to reduce opioid prescriptions, they worked with pharmacists to ease chronic-pain users down to more reasonable doses, despite resistance from drug users.
The health care teams used withdrawal management treatments and also incorporated counselling to help people transition to safer doses.
Now, prescribers are treating chronic pain patients with non-opioid or opioid-like chemicals.
“If this treatment plan fails, the patient may require opioids; however, it is uncommon to see a patient started on oxycodone today as there are other opioids available that are less likely to be abused and/or have less street value,” Mr. Gauthier says.
Dr. Lionel says, despite the risks of harm, villainizing opioids in totality can be counter-productive. He believes in the power of opioids for good and says they may be necessary at times, such as up to a week after a surgery.
“Don’t be fooled. In the short term, (opioids) are an excellent medication, but they need to be used judiciously,” he says. “You need to find the middle ground.”
Over the medium term, a few people can do well using opioids, but into long-term usage, very few people do well with opioids, in his experience. Users need a very structured program so medical professionals can intervene if they begin to lose control.
“That can save them from the dreadful disease that is opioid use disorder, or what we used to call addiction. That is a life-threatening disease.”
Chapter three
Harm reduction kits are made available through public health and many of the Island’s First Nations health organizations.
Although opioid-related deaths have steadily increased in recent years, the COVID-19 pandemic has brought a never-before-seen ferocity to the rise.
The restrictions to stay home and avoid in-person interactions with others has meant more drug users consuming their supply away from the care of medical professionals through resources like supervised consumption sites.
A report from the Canadian Centre for Substance Use and Addiction (CCSA) shows the pandemic has also brought a decrease in the numbers of people using drug checking services, homeless shelters, outreach programs and other harm-reduction services like needle exchanges. For services that continue to operate, many have faced staff shortages and, in some cases, COVID- 19 outbreaks.
Pandemic-related border closures have meant disruptions to the international illicit drug supply chain. The CCSA report shows that illicit drug operations have sought alternative, unknown producers to fill the demand.
Drug prices for certain substances doubled or tripled in some regions, the report continues. In places without price increases, some users have reported that their drugs have become ‘weak,’ or that they have been cut with other substances. This has coincided with more unexpected side effects.
This adds to a growing trend in surveillance data about illicit drug supplies: drug toxicity is steadily increasing, and has only worsened since the onset of the pandemic.
As drug toxicity rises, there’s another threat: naloxone, the easily accessible overdose reversal drug, is not as effective against overdoses from fentanyl and its higher-potency analogues.
While it once could reliably save lives until paramedics arrived, naloxone may no longer be able to counteract every overdose.
The phenomenon of opioid tolerance in longterm users becomes a major problem in the context of supply disruptions. Within a few days of not consuming opioids, the user’s tolerance begins to decrease. If they try to take the same dose as when they used regularly, it could kill them.
Add all of the pandemic disruptions to the growing toxicity in illicit drug supplies and the result is a foundation for a surge in overdose deaths.
That’s exactly what began to emerge on Manitoulin Island, and across Canada, last year.
Distribution of opioid-related deaths by age
Pre-pandemic cohort (March 16, 2019 – December 31, 2019) – Pandemic cohort (March 16, 2020 – December 31, 2020)
Public Health Ontario says more than 2,400 people died in the province in 2020, up 60 percent from the 1,517 deaths reported in 2019. Fentanyl was involved in 87 percent of opioid deaths during the pandemic, the report continues, up from about 75 percent before the virus. The highest rates of opioid deaths during the pandemic were all in Northeastern Ontario, including the PHSD area. Further Public Health Ontario data show PHSD’s rates of opioid deaths were three times higher than the whole province before the declaration of the pandemic on March 11, 2020. The gap has only since widened.
The Sudbury-Manitoulin area saw 11 opioids deaths per 100,000 citizens in the 15 weeks before the pandemic declaration, which rose to 14 per 100,000 for the 15 weeks after that date.
Deaths involving some type of stimulant in the health district grew by an alarming 200 percent between 2018 and 2020, while Ontario as a whole only saw a 19 percent increase. The vast majority of stimulant related-deaths in the Sudbury-Manitoulin area in 2020 also involved opioids.
Canadian studies have shown at least 40 percent of people reporting worse mental health during the pandemic. At the same time, many of the usual support options and healthy social outlets have closed due to the virus.
“It’s a perfect storm right now. Sports, for many young people, have been a salvation. When you can’t participate in sports and you live in a small town, you have to make your own fun,” says Mr. Jocko, the Anishinabek Nation policy analyst, who offers Little NHL as an example of an all-encompassing event for whole families.
The opioid crisis is a personal passion for Noojmowin Teg executive director Danielle Wilson, who took over the health agency’s top spot last year. She is from British Columbia, where the overdose epidemic has had profound effects ahead of most of the country, especially within First Nations.
Drug-toxicity deaths had been on a longterm decline in BC until the start of COVID-19, when fatalities rose 61 percent in a month— from 70 in February to 113 in March 2020.
Ms. Wilson says Manitoulin’s rate of opioid prescriptions has remained relatively steady during the pandemic but the number of overdoses has skyrocketed.
“We’ve been calling it a co-pandemic. More people have been impacted by opioids than COVID here on Manitoulin. If we could only mobilize those same efforts from COVID but for opioids, we’d be in a great place,” she says.
Distribution of opioid-related deaths by sex
Proportion (%) of men among opioid-related deaths increased from:
During the pandemic, there has been a statistically significant shift towards more opioid-related deaths occurring among males. Specifically, 70.8% of deaths (823 of 1,162) in the pre-pandemic cohort were among males, rising to 76.3% of deaths (1,565 of 2,050) in the pandemic cohort (p<0.01).
Care providers have seen mixed results in the numbers of people accessing their services over the past year. While Northwood Recovery has experienced an increase in its client numbers, Dr. Lionel says he has seen a drop in his addictions medicine patients.
One potential reason, he says, may be the introduction of the Canada Emergency Response Benefit (CERB)’s $2,000 monthly distributions for those impacted by COVID-19. Because addictions can override the decision-making centres of the brain, many may have bought drugs before covering their basic needs. “There’s probably some well-paid dealers out there now,” Dr. Lionel says. “I understand CERB was necessary and it’s helped a great number of people, but it’s also caused a lot of harm.”
Dr. Poenn, the Island doctor and coroner, says the growing opioid crisis is of great concern to him and his fellow medical care providers.
“The numbers tell a pretty clear story in terms of the number of people dying with opioids in their system, though it doesn’t break it out in terms of accidental and intentional (deaths),” he says.
Drugs continue to drive emergency department visits, principally because of alcohol, but there are increasing cannabisrelated problems among younger users especially, as well as combinations of multiple substances.
Opioids tend to cause higher rates of skin infections and diseases in people who use needles. Dr. Poenn has seen several cases of flesh-eating disease, a group A strep infection in a patient’s deep tissue, because of needles. He has also seen people with spinal abscesses and infections between their back vertebrae.
“Those infections are difficult to manage and can lead to lots of longterm problems,” he says.
The situation appears bleak. People are dying. Leaders working on the ground are exhausted and low on resources. Criminal drug traffickers continue to target vulnerable people and the he. alth impacts of opioids are spilling over into all areas of the health system.
In many ways, Manitoulin Island is paralyzed.
Chapter four
Sergeant Cooper of the Wikwemikong Tribal Police Service and his fellow officers are continually having to cope with drug dealers, almost always from the GTA, infiltrating the community.
At the same time as the opioid crisis grows, other problems like violent crime are also rising on Manitoulin Island. More and more families are facing the impacts of the crisis among their loved ones.
It has been a striking contrast for Inspector Slaughter, of UCCM Police, who moved to Manitoulin from Ottawa late last year.
“I love the environment here; it’s beautiful, but it has been infiltrated by those making money off of those with addictions,” she says. “But this is how (criminals) operate. They have groups of people involved in organized crime that run to the specific areas. This happens all over; no places are immune.”
According to police forces, the drug supply on Manitoulin mostly begins in the Toronto area and moves north into towns and First Nations.
But it doesn’t stop at this latitude. Even remote Northeastern Ontario communities as far north as the James Bay coast are seeing criminals enter their midst, says Det. Sgt. Fox of WTPS.
“I’ve heard information of (drug dealers) going up to Moose Factory by catching a train. Again, these are people that are known to be linked to Toronto through investigations,” he says.
There’s a lot of incentive to sell narcotics in places like Manitoulin. In addition to the presence of many vulnerable individuals, the black market for drugs in the North can be much more lucrative.
“It’s primarily, from what I understand, about the markup and how they sell their product. Drugs here sell for about five times what they sell for in Toronto,” Det. Sgt. Fox says.
When they infiltrate smaller communities, criminals often seek exploitable people to further their operations. These are often people who had already been using drugs and the criminals will use them to set up local distribution points. These locations tend to change frequently to thwart detection.
Exploiting vulnerable people for profit is considered human trafficking. Det. Sgt. Fox says that, although he has not seen it first-hand, he has heard reports of human trafficking of a sexual nature, too, in which victims will exchange sexual services or explicit photographs to cover debts or to obtain drugs.
In many ways, drug traffickers have infiltrated the very social fabric of Manitoulin Island, especially in First Nations, whose health staff, band leadership and police services are working steadily to protect their people as best they can in the face of unprecedented challenges.
In some cases, criminals have gone beyond coercing community members to work for them and have instead taken over the homes of vulnerable individuals such as elders.
This newspaper has asked OPP about the presence of home takeovers and human trafficking in its service area. Manitoulin OPP detachment commander Inspector Megan Moriarity says, “these issues are present across the province.”
She says the detachment works with policing and community service partners to address safety issues, but does not directly address the presence of such behaviour in the detachment area.
The Expositor has unsuccessfully asked Island police forces for an estimate of how many people are involved in the illicit drug trade on Manitoulin.
Exploiting vulnerable people for profit is considered human trafficking. Although he has not seen it first-hand, he has heard reports of human trafficking of a sexual nature, too, in which victims will exchange sexual services or explicit photographs to cover debts or to obtain drugs.
A history of OxyContin
Purdue Pharma’s OxyContin, a painkiller that debuted in 1996 as a long-acting oxycodone analog, is among the most notorious opioids.
Within a few years of the drug’s release, Purdue Pharma knew that OxyContin was connected with a rise in addictions but the company did not act on that knowledge. These facts are in the public record through investigative journalism reports, court cases and leaked internal documents.
Purdue continued to aggressively push OxyContin toward physicians, including offering bonuses to doctors who prescribed more doses of the drug. Other opioid-selling pharmaceutical companies mocked patients who had developed dependency, even as they began to understand that their products were not as benign as intended.
One of OxyContin’s serious flaws was the recommended dosing schedule. Previous opioids often used an eight-hour dose interval but Purdue recommended a higher dose on a 12-hour schedule instead. OxyContin loses half of its strength four-and-a-half hours after ingestion.
Advocates have since realized just how disastrous this decision was. After 12 hours, a majority of prescription holders would already be starting to feel the effects of opioid withdrawal; taking another pill at that time would strengthen the reward circuit inside the brain.
Being an officer in a small First Nation community requires forming trusting relationships with the people they serve.
“It’s become such a vicious circle that I don’t know how to tackle it anymore,” says a member of the leadership of an Island First Nation, who asked The Manitoulin Expositor to withhold their name because of the potential risk to their safety. “I’m so tired, going out and trying to deal with these people. You put your life at risk when you go out by yourself and there’s no police there.”
The leadership member says they have begun to see elders selling their prescription drugs for profit, and that some of the Islanders involved in the drug trade are people who were once fierce anti-drug advocates.
Communities are already experiencing frequent instances of lateral violence (when people direct their aggressions toward their friends and neighbours, rather than at the main problem). Besides causing further, unnecessary harm, these incidents can distract people from addressing the root causes of the crises at hand.
As these pressures continue to erode community trust and safety across Manitoulin Island, a new crisis is silently taking hold.
Fear.
Criminals intimidate community members and neighbours against reporting their activities and many Islanders are now reluctant to report criminal activity. This only makes the fear cycle grow stronger.
The traffickers’ strategy is working. But it doesn’t have to be.
“The fear in the community is something that can hamstring our efforts when we don’t get the information we need,” Inspector Slaughter says. “We really want to inspire the community to continue keeping us informed.”
But community members can also get discouraged when they don’t see immediate results from their tips. In the view of many people, governments and law enforcement agencies don’t seem to be doing anything to stop the bad actors from destroying their friends and family.
That feeling can be frustrating, says Inspector Slaughter, but she says tips are crucial for police to build their cases toward future search warrants and arrests.
“The reality is, we have to play within the rules of law. We can’t just necessarily go on information like that; we have to gather information and put together a solid case that can go before the courts,” she says.
Risk of addiction
Scholars believe genetics make up roughly half of one’s risk for addiction, a phenomenon visible in studies of twins raised in separate households.
The traits most closely associated with increased risk of addiction, according to a 2017 Virginia Commonwealth University write-up, are impulsivity, sensation-seeking and difficulty coping with stress.
Those who live with conditions like anxiety and depression are also at higher risk for addiction. Some may turn to substances initially for temporary relief from mental illness, but once addiction sets in, one’s mental health tends to worsen.
The younger someone is when they begin to use a narcotic, the higher their chances of developing an addiction, and the greater the chance for long-term mental effects as the brain does not mature until one’s mid-twenties.
Det. Sgt. Fox of WTPS also sees the frustration from community members when police cannot stage an immediate response, but he says many of the public’s reports would not meet the evidence threshold to proceed in court.
Especially in small, rural and Northern communities like on Manitoulin Island, it is often ‘common knowledge’ which houses are connected to drug activity and which individuals have a role in trafficking, which can make it harder for neighbours to be patient for the official process to unfold.
“As a law enforcement organization, the OPP’s role in this crisis is to investigate opioid-related incidences with an acute focus on the apprehension of those who produce, import and traffic illegal drugs,” says Inspector Moriarity. She says the provincial police service is committed to direct “adequate resources” toward addressing the root causes of mental health and addictions.
To further encourage the public to submit tips, UCCM Police has begun a public appeal for information on any suspicious activities, including a stranger hanging around one’s neighbourhood for a long time, high levels of traffic visiting a home every day, people arriving at or leaving homes at unusual times, or several people who appear to be working together and displaying suspicious behaviour.
Further complicating UCCM Police and WTPS’ steady efforts against drug traffickers is the fact that Ontario does not recognize First Nation police forces as essential services. As such, they do not receive the same levels of funding and resources as agencies such as OPP or even municipal police forces.
The Expositor has explored this issue in the series, ‘Defunded from day one: Part I of a series,’ though the project ended earlier than expected when the featured police chief had to step down from his position.
The police actions to remove drug dealers from Manitoulin and prosecute them are important, urgently needed and, some would argue, a necessary step to solving the overdose crisis on the Island.
But those efforts will never be enough.
At Island-wide leadership meetings, mayors and reeves often listen to the situations their First Nation partners are experiencing and learn a great deal about the extent of the drug problems on the Island.
“As a mayor, I’m not involved in the town’s administration directly. It’s actually against the law; I have to delegate that to my CAO and staff. We determine policy but don’t get actively involved. It’s different for First Nations. Linda (Debassige, ogimaa-kwe of M’Chigeeng) is the chief, but also an administrator. She’s worked off her feet in terms of doing her job, a well as trying to be the political leader,” the mayor says, noting that the Island’s First Nation leaders often cannot attend every Island leadership committee meeting because their time is stretched so thin.
The fear in the community is something that can hamstring our efforts when we don’t get the information we need. We really want to inspire the community to continue keeping us informed.
Eddie’s story
Eddie Gough’s lifelong struggles with mental health and addictions have come full circle. He now seeks to help those in his former position in everything he does.
Eddie Gough was born in 1979, still within the 60s Scoop, when government child services removed thousands of Indigenous children from their parents at birth.
When he was six months old, he was adopted into a white family in south Mississauga. He could recognize that he was different from an early age and often struggled with his identity. He knew he was Indigenous but didn’t know what that meant beyond stereotypes and being bullied more.
“That kind of pushed that self-hatred and shame within myself; I considered being Native as something that was wrong or ‘less than,’ which really affected my self worth,” he said.
His adoptive parents were not overly affectionate and Mr. Gough developed abandonment issues. He said his brain wanted love but also told him he was unworthy of love. This led to rage and behavioural problems.
He eventually entered group homes but ran away a few times, choosing to live on the street, worsening his feelings of abandonment. In his early teens, he began to use drugs and alcohol socially.
“Instead of meeting that sense of belonging from my family who, in my mind, abandoned me, I started looking for it through my social networks. But the people I was around were definitely not the best influences and also had their own struggles,” he said.
Into his 20s, he got his life together a bit and worked for several years, but he still struggled with depression as the people he knew from school were all beginning their adult lives.
“I very much felt like I was an adolescent trapped in an adult body. I didn’t have the tools to progress,” he said.
In his late 20s, he first used cocaine and quickly developed an addiction. It offered temporary relief from his negative feelings and shame.
Mr. Gough tried his first opioid after a dentist removed his wisdom teeth and prescribed him Percocet.
“I already had a heavily addictive personality. As soon as I took this, I thought it made all my emotional pain go away for just a bit. That captured me very quickly,” he said.
Eddie Gough is constantly learning about his First Nations ancestry. He wears the moniker of the bear clan proudly.
Percocets turned to OxyContins as his daily use grew. He knew there was a risk of overdose and other harms, but he always believed he was in control and wouldn’t allow it to get that bad. After all, OxyContin was regulated and supposed to be relatively safe, and he wouldn’t dare take anything harder than that.
Until he tried heroin.
Before long, he had gotten onto fentanyl.
“At that point, my addiction was so far gone and I had lost everything. I was basically trying to kill myself with drugs. Even among my opioid addict friends, they had limits. I ultimately was still carrying my mental health issues, shame, failures and abandonment,” he said.
He survived an overdose and tried treatment three times, but still couldn’t break the cycle. His childhood best friend, who also grew up in a traumatic household, was struggling just as badly. The two both had suicidal ideations and they made a pact to end their lives together.
“We picked a day, we knew how we were going to do it. But then something within me, something very spiritual, said ‘you can’t do this.’ That very day, I told him I had to back out and I went to CAMH (the Centre for Addiction and Mental Health), told them I was suicidal and they started giving me crisis counselling,” he said.
His best friend didn’t join him. Mr. Gough was one of the first people who found his body.
That brought extra trauma and CAMH increased his crisis counseling. Workers connected him to an Indigenous social worker who introduced him to ceremonies, traditional medicines and taught him about his heritage.
“That was my healing. I had tried all sorts of western therapy my whole life: psychologists, psychiatrists, counsellors, every mental health medication under the sun and AA. But from that point on, I slowly started removing the addictions from my life,” he said.
He got involved with ceremonies through volunteering at Anishnawbe Health Toronto and his social worker enrolled him into a social service worker program at First Nations Technical Institute in Tyendinaga.
It was the first time he had spent more than a passing visit in a reserve and he was terrified, because his knowledge of First Nations was based on stereotypes.
The community embraced him and offered him their support, such as encouraging him to discover his roots in Wiikwemkoong. The school sent a small production crew along to make a documentary of his trip to the annual cultural festival, where he met his biological brother and sister.
“It was one of the most powerful, amazing experiences of my life, spiritually too,” he said.
The documentary turned into speaking engagements and Mr. Gough travelled widely to share his story to help others who may be struggling with self-worth and might be at risk of addictions.
He made a close friend from Whitefish River First Nation who introduced him to Gwekwaadziwin Miikan, Aundeck Omni Kaning’s land-based treatment program. He applied to work there as a counsellor and moved north, despite only knowing a handful of people.
May 2021 marked his two-year anniversary at Gwek. “At this point of my journey, I’m still healing from the land and using it to understand my own traumas and struggles, and learning to channel that into something that helps me relate to and understand others,” Mr. Gough said.
Chapter five
Pharmacists like Chris Gauthier are often on the front lines of the opioid crisis.
Simply criminalizing the sale, possession and consumption will not solve the problem. It may be a key part of the solution but law enforcement cannot eliminate the drug crisis on its own.
The notion that police could end these social ills was a pillar of the ‘War on Drugs,’ a US-led campaign first begun in 1971 under the Richard Nixon presidency that has since spread across the world.
That war is now widely dismissed as an abject failure, including in the view of the Global Commission on Drug Policy. It published a report 10 years ago, arguing that the campaign “has had devastating consequences for individuals and societies around the world.”
“Drug policies and strategies at all levels too often continue to be driven by ideological perspectives, or political convenience, and pay too little attention to the complexities of the drug market, drug use and drug addiction,” its commissioners wrote in 2011.
“We’re not winning (the War on Drugs). There’s more people dying every day, no matter how much policing, interdiction or border control. You’re never going to stop drugs. … If you can smuggle a million doses of carfentanil in a container as big as a packet of sugar, how do we ever get it under control? You can’t. It’s not possible,” Dr. Lionel says.
The ability for drugs and violence to destroy families “is a very sad circumstance and it’s a high concern for us as a police organization,” says Det. Sgt. Fox.
“But at the same time, this is not (just) a police issue. This is an issue for every agency to come together, to band together, to engage in dialogue and come up with meaningful, lawful strategies we can impose that will help mitigate this to some degree,” he says.
Mental health experts consider substance use disorder to be a mental illness and, in many ways, a social problem.
For this reason, communities have to collaborate and innovate to identify potential solutions that will work within their unique circumstances.
Dr. Lionel says instead of spending money on drug enforcement, those dollars should go toward education and support for people who develop substance use disorders. He urges lawmakers to decriminalize drug possession, because the illegality is what has caused illicit markets to emerge, but says there is currently little political will for such measures.
“Maybe one day it will happen. In the meantime, we need to come up with innovative options for helping people who want to use and don’t want to get involved in the toxic supply,” he says.
We’re not winning (the War on Drugs). There’s more people dying every day, no matter how much policing, interdiction or border control. You’re never going to stop drugs. … If you can smuggle a million doses of carfentanil in a container as big as a packet of sugar, how do we ever get it under control? You can’t. It’s not possible.
Dr. Lionel, as his patients call him, provides consultation and educational services about drugs and has spoken at Island conferences in years past.
While the War on Drugs has not had the lasting impact of fixing the problem, it has deeply imprinted negative impressions of drug users in the minds of many people. This means drug users face heavy stigmatization and barriers to getting help.
An oft-repeated phrase is that drug users have chosen to ‘throw their lives away’ and don’t deserve the government’s support. This, despite a 2018 CCSA study that shows substance use cost Ontario $14.7 billion in 2014 alone (that’s more than $1,000 per citizen), a number that would certainly have risen as the opioid crisis has worsened.
That annual price is a mixture of health care costs, the criminal justice system, lost productivity and other direct impacts.
The stereotypes persist nevertheless and, in addition to making the crisis worse because drug users have to turn to street supplies, it also creates barriers for drug users to get support.
People who do not support harm reduction programs often cite the importance of personal accountability and say the onus is on drug users to cut out their compulsion.
But when considering the ongoing costs of substance use as well as the history of weak oversight of pharmaceutical companies’ falsified safety assurances, the argument for systemic support gains some merit.
While some people indeed start using drugs recreationally, a 10-year US data review of 600,000 heroin users found 79.5 percent of respondents had first gotten involved with opioids by abusing a prescription drug.
Nearly 10 percent of Canadians 15 or older in 2018 said they had used a prescription opioid for non-medical purposes. Other studies have reported that between three and 29 percent of patients with opioid prescriptions for chronic pain misuse their drugs in some way.
“The medical portion of this equation were convinced that (Oxy- Contin pills) were much safer and could be doled out like candy,” says Mr. Jocko, the Anishinabek Nation federal health policy analyst. “They were going to be the messiah of all medications.”
That turned out to be dangerously untrue.
Synthetic opioid painkillers grew popular among doctors in the 1990s. Drug makers had adjusted existing medications to offer more powerful or longer-lasting effects and they pushed hard to get their new era of drugs into patients.
Sheguiandah resident Aaron Case, who vowed to get clean after nearly dying of an overdose, knows just how debilitating the stigma can be, even for people trying to recover. He says he almost gave up on opioid replacement therapy because of scorn from members of the public and some pharmacy staff.
“I kept falling through the cracks all the time. The pharmacist would treat me like shit when I would go in to get my (suboxone) … I didn’t even want to go to get my medications because I felt degraded,” he says. “There’s still certain people, they don’t say it, but I know they look at me differently even though I’ve changed my life around. People judge people way too easily.”
Nevertheless, he remained committed to recovery and now helps others to heal from their own substance use disorders as a land-based counsellor at Gwekwaadziwin Miikan in Aundeck Omni Kaning.
There are several factors that increase one’s chances of developing a substance use disorder, including their genetics, environment, other medical conditions and the age when they first use. The way a user consumes drugs can also play a role, as injections and inhalation are more potent and liable to cause a use disorder.
Opioid maintenance treatment options from
best to better
Sublocade is an injection that lasts for a month, eliminating daily pharmacy trips, while Probuphine consists of small rods that go under the patient’s skin and last for six months.
Suboxone contains buprenorphine, which blocks opiate receptors and reduces a person’s urges, and naloxone, which helps reverse the effects of opioids. Together, these drugs work to prevent withdrawal symptoms associated with an opioid addiction. Suboxone comes in film or tablet form.
Methadone is a long-acting opioid used to replace the shorter-acting opioids that someone may be addicted to, such as heroin, oxycodone, fentanyl or hydromorphone. Methadone powder is dissolved in liquid and taken once a day.
All options work best when coupled with addictions counselling.
At the community level, withdrawal management services and opioid agonist therapy are key tools in easing people away from illicit and dangerous drugs. But finding locations for such clinics is often challenging because they must try to be as accessible as possible for drug users while also managing community members’ concerns about real or perceived safety risks.
Northeastern Manitoulin Family Health Team executive director Judy Miller has long been a proponent of having such services available on Manitoulin Island, despite a sometimes- challenging history of these programs.
In early 2013, Northeast Town’s council voted to bar Dr. Bryan Dressler’s methadone clinic from operating in the heart of downtown on Water Street. The public had expressed safety concerns after a fight had broken out along the sidewalk.
Mr. Gauthier, the Little Current pharmacist, says methadone and similar therapies can be very effective in getting drug users off of the dangerous street supply, but he agrees that the downtown strip was not an ideal location for such services.
“It created a negative stereotype of the clients that were there to get help. It was not the best choice of location and it would lead to a loss of anonymity and patient confidentiality,” he says.
Dr. Dressler said he would leave Manitoulin after council voted to shut down the operation, putting his patients’ health in jeopardy.
Ms. Miller formed a group with Naandwechige-Gamig Wikwemikong Health Centre, Noojmowin Teg and M’Chigeeng Health Services to keep the doctor around. She offered him space in the family health team building as a safer location that respected patients’ privacy.
Dr. Dressler ultimately left the Island and a southern Ontario service that later served Wiikwemkoong also pulled out. This ultimately led to the introduction of Dr. Suman Koka’s Northwood Recovery practice, which includes several aspects of addiction medicine and rehabilitation.
Dr. Koka also offers on-call services for the rapid access to addictions medicine bed at MHC for people in immediate crisis. Island health providers are working on a more permanent solution for those services, which can be challenging to implement in rural locations because of the travel required to access urgent services.
The health providers’ goal has always been, as much as possible, to integrate the care within existing practices as much as possible, to offer wraparound services to patients. Without this mindset, the programs cannot reach full effectiveness, according to a number of studies over the past decade.
In Wiikwemkoong, for instance, Dr. Koka’s clinic operates in a building that also houses a traditional healer and a wellness worker. Ms. Miller says there are 168 active Northwood Recovery patients on Manitoulin Island.
Pills like hydromorphone, while a useful tool to deal with pain, are highly addictive.
Ms. Wilson, the executive director of Noojmowin Teg, has collaborated with her primary care team and member First Nations, both of which said mental health and addictions were urgent concerns.
“I’m pleased to know Noojmowin Teg’s primary care team is just as interested and passionate about embedding (mental health and addictions services) in their practice as well. It’s whatever we can do to help out our communities,” she says.
In response to that shared concern, the physicians and nurse practitioners, behind leader Dr. Erin Peltier, all enrolled in addiction medicine training. This will allow the team to integrate these services in a patient’s regular check-ups to create an accessible, holistic care model that’s easier to access.
In addition to being able to prescribe opioid therapy drugs like suboxone, Noojmowin Teg will offer the wrap-around services of metal health supports, health and wellness programs—including those specifically for children and youth— family healing, fetal alcohol spectrum disorder support and traditional medicines.
“We’re not quite at the state of opening our doors to see clients (for the addictions program) just yet; this needs to have strong partnerships with our First Nation communities as well,” Ms. Wilson says.
The goal is to start small pilot sites with Island First Nations this summer and expand from there.
“The most important thing about addiction medicine is that we want to make sure there’s no gaps in any of the services, in terms of referrals to the program and then follow-up care, says Ms. Wilson.
Although the Noojmowin Teg team expects this innovative program to improve health outcomes, the program is not receiving any funding. The health centre is paying for it with internal resources because of its potential to change lives.
MHC staff are working to establish clear pathways “between the hospital, primary care and support services like community withdrawal management and community mental health and addictions workers, to support these patients in a full continuum,” says Melanie Stephens, MHC’s manager of clinical innovation and partnerships.
Mr. Gauthier says pharmacists and health care providers alike now spend more time to educate patients, particularly those at higher risk of developing addictions, about the potential dangers of opioids. These warnings also appear on prescription vials.
“(Pharmacists) are often the first health care professional that a patient will see when prescribed an opioid and we are armed with the knowledge required to warn patients of the risks,” says Mr. Gauthier.
Health providers also connect patients with harm-reduction services like the overdose-reversal drug naloxone, information on needle exchanges and the locations of biohazard bins for used needles.
Ms. Stephens says Manitoulin Drug Strategy is working on a Manitoulin version of Sudbury’s opioid poisonings response plan. That city’s Community Drug Strategy, published in 2019, details what each community safety partner must do when there is a sudden outbreak of opioid deaths.
The plan’s prospective outcome includes monitoring anecdotal data from Island residents to generate immediate drug alerts when dangerous substances may be circulating on Manitoulin, alerting drug users before toxicological testing confirms those reports.
The local response framework planning process involves paramedics, MHC, primary care providers, law enforcement, mental health and addictions workers and local governments, both First Nation and municipal, says Ms. Stephens.
Jean & Andrew’s story
Andrew was a kind, loving and caring individual who began to struggle more and more with substance use and anger issues until his death in Little Current last year of a fentanyl overdose. He was in his mid-thirties.
The Expositor has agreed to change the names in this story because there are still tensions within the family about Andrew’s struggles and his death during the rising opioid crisis on Manitoulin Island.
“I knew he had been taking this, that and the next thing, but he was a really good, hard-working man. He lived in the Sudbury area and worked good jobs, but he never seemed to have any money. The way it ended up, he had nothing,” his mother, “Jean,” told The Expositor.
Andrew was never the most confident of kids growing up. Jean attributed part of that to her former husband’s reportedly controlling behaviour. She still carries bitterness toward him over their son’s fate.
“His father just didn’t have the fatherly touch to him,” Jean said. “Even in his 20s and 30s when he’d help his dad, he never received so much as a ‘good job’ from him.”
Andrew was involved in a bad car crash in his younger years and received dozens of OxyContin tablets from a doctor for his pain.
“I asked to see what the doctor had given him and I was furious, I was shocked. He’s just a kid and they said to take the pills two or three times a day; I thought they could have given him a third of that amount and then checked back. That started the ball rolling really badly,” Jean recalled.
When Andrew was in his late teens, after leaving high school, his father said that he would be driving his son down to Barrie, where he would have to figure out life, just as the father had chosen to do when he was 16.
“(Andrew) just looked at me with tears in his eyes because he had never been away from home. And he did it—the next day, his father packed him up and took him down,” Jean said. “I think if someone had done that to me, it would have just destroyed me.”
Andrew eventually returned north to the Sudbury area and visited his mother every Friday to help her around the house. He moved back to the Island full-time four years ago.
Over the past year, Andrew struggled more than before. He was asking his mother for money almost daily, often first thing in the morning. He would also get angry, though never physically violent, at any frustration he faced.
And while he had once been quick to repay any loans, Jean began to accept that she would never see her thousands of dollars again. Her son also fell behind on payments for his beloved truck.
She said Andrew’s father never saw the problematic behaviour in his son.
This past fall, Andrew met with friends to mourn and celebrate the life of another friend who had passed away. He came home in the middle of the night on a Wednesday and exhibited bizarre behaviour, such as asking his mother incredulously why she was asleep in bed at 4:30 am.
The next day, it was even worse. He came home at 8:30 pm and gave a weak knock on the door, then took a long time to enter the house.
Jean remarked a couple of times that he was home rather early, but he never responded. She knew he had been at another memorial party after a long day of work, and figured he might have been exhausted or had too much to drink, so she let him go to his room.
It was the last time she saw her son alive.
AUTHOR’S NOTE: The next two paragraphs contain disturbing details that may be difficult to read.
The next morning, her son didn’t wake at his normal time, which Jean thought might have meant he was exhausted and choosing to sleep in. But by the early afternoon, something was clearly wrong.
“I opened the door and he was on the floor. I didn’t want to panic but I just wanted to fall apart. I called his name, told myself I had to get calm, and touched his back. He was cold,” she said.
The hours around her son’s accidental fatal overdose haunt her to this day.
“I feel like we could have done something. I mentioned a few times, ‘be careful, because (fentanyl) is around now.’ I had never even heard of it before. It makes you feel so bad that a young person, they have everything to live for but are troubled in so many ways. You do what you can but I often regret not going in to check on him that night and ask if he was okay,” Jean said.
Instead of supervised consumption sites, she said more emphasis should go toward recovery and treatment options that deliver effective results, and urged people to have compassion and to be caring, especially within their own families.
“There’s other parents who have gone through this; it’s hell on Earth,” she said. “He knew I was probably the only person who was really there for him. That must be a terrible feeling. It’s really sad that there wasn’t more family support because different people had heard that this was a problem. But of course, when they saw him, he would usually look fine.”
Jean also sought answers of why drug producers make knowingly toxic substances and why, despite often knowing who the drug dealers are, police have such a hard time getting rid of them from the community.
Chapter six
Officers Island-wide have seen their roles change in the community as they respond to ever-increasing mental health and addictions calls.
Treating opioid use disorder effectively requires trust between the provider and the patient, says Dr. Peter Menzies, a registered social worker who specializes in Indigenous mental health, addictions and trauma, but it also requires the right kind of program. If they’re not well-designed, treatment programs can be more than just ineffective— they can be dangerous.
Many publicly funded treatment programs only last a month or less, a concerning model for Mr. Case, who says the ideal amount of time is at least two months of steady support and, ideally, supportive aftercare, to make the treatment stick. He beat his substance use through a live-in program of six weeks, followed by aftercare.
“The government-funded programs are a joke because you just start feeling good at that point. You need that 60 to 90 days to really understand what’s going on and get your feet back on the ground. With the 21- and 31-day programs, you just see relapse after relapse,” Mr. Case says.
Dr. Lionel says programs that require sobriety before starting have led to high-profile deaths in recent years, including Phillip Seymour Hoffman and Heath Ledger. This is because tolerance fades quickly, so a relapse is much more serious.
“If you slip up and use anything like you were using before, you will die,” he says. The individual has to be willing and receptive to getting help in order for these programs to work best, says Dr. Lionel, who agrees that aftercare with follow-up check-ins and counselling support is crucial once a patient returns to an environment that’s full of triggers to use again.
Dr. Lionel says the best options for recovering patients who have gotten their intake down to a low dose of suboxone are Sublocade or Probuphine, both long-term options that eliminate many of the barriers from methadone, such as daily triggers and stigmatization when a user picks up their doses.
Sublocade is an injection that lasts for a month, eliminating daily pharmacy trips, while Probuphine consists of small rods that go under the patient’s skin and last for six months.
Mr. Case has the distinction of being the second Probuphine user in Canada and says it changed his life.
“I had my life back. I could work, I lived a normal life and I didn’t live like I was still in the shadows of addiction, where I’d go to the pharmacy every day and get that constant reminder,” he says.
The problem with Probuphine is that it involves a minor surgical procedure, something many physicians are uncomfortable performing, says. Dr. Lionel. He is one of the Canadian trainers for that operation and he travels across the country educating doctors.
“I don’t think (Probuphine) has had the traction I’d like it to have; I’d like to see more people get on board with this,” he says. “The patients who are on it are very happy and do very well.”
I had my life back. I could work, I lived a normal life and I didn’t live like I was still in the shadows of addiction, where I’d go to the pharmacy every day and get that constant reminder.
Chapter seven
Paul Myre, chief of paramedic services with Manitoulin-Sudbury District Services Board, says understanding the full scope of the epidemic is a complicated matter.
Increasing numbers of people are beginning to see the opioid crisis for what it is: a social ill that will require compassionate, effective solutions to deliver results.
“There’s so many pandemics in our communities, whether diabetes or now, illicit drugs. It all goes back to the resources and capacity of the local communities to be able to mount these comprehensive programs and interventions before they start,” says Mr. Jocko, of Anishinabek Nation.
First Nations and non-Indigenous communities alike are finding themselves overwhelmed by the magnitude of the problems, Mr. Jocko says, and many lack adequate resources to make meaningful progress on the issues.
“It’s always been a capacity problem. This became a huge problem overnight and now we need prevention programs, mental health workers, addiction workers and we also need treatment centres. For a very long time, we’ve had chronic shortages of all of those things,” he says.
Mental health medications can help in getting an individual stabilized before starting therapy but many people stay on those drugs long-term because they cannot access effective treatment. Those drugs come with their own problems after longterm use.
Therapy programs are not equally accessible among all people. Better access to publicly funded mental health services would be a great advantage, Mr. Jocko says, because First Nations are often limited in the options they have for health care.
That lack of options, he says, may have contributed to why First Nations appear to struggle with higher rates of addictions. Many Indigenous people in Canada do not have access to third-party health care, such as through an employer, so the only drugs and services they can access are through Canada’s Non-Insured Health Benefits program.
“The prescriber, pharmacy and consumer are very limited to what they can access and what’s covered. That definitely would have played some part in all this,” Mr. Jocko says.
Mayor MacNevin of the Northeast Town agrees that Manitoulin is “woefully under-represented” in mental health services.
It’s always been a capacity problem. This became a huge problem overnight and now we need prevention programs, mental health workers, addiction workers and we also need treatment centres. For a very long time, we’ve had chronic shortages of all of those things.
There are a growing number of examples of successful youth prevention programs on Manitoulin Island, particularly in First Nations, that give young people the skills they need to foster resilience and avoid making harmful choices. These do not replace the immediate need for robust mental health services but they may help reduce the demand for such programs in the future.
UCCM Police ran a summer leadership camp for Anishinaabe teens in 2019 that included team-building activities, traditional teachings and conversations with elders, but also allowed youth to build positive relationships with law enforcement and paramedic services, who taught them first aid and how to use a naloxone kit.
Wiikwemkoong is beginning to implement a $4 million grant for a youth program to build resilience among students, their families and the community, as well as strengthening the children through mental health supports. Other Island harm-reduction programs in recent years include youth sports programming that also delivered education on the harms of smoking.
Targeting youth can be very beneficial because they are developing a sense of self and are more vulnerable to identifying with harmful influences. Had programs like this been in place over past decades, says Mr. Jocko, the mental health and addictions crises might not have been so disastrous.
“The governments of the day have never put a lot of emphasis on prevention. Our schools have been crying for mental health workers for decades and the governments of the day would never fund them; now, we have an epidemic of mental health issues,” he says.
While many harm-reduction studies have indicated that it is most effective before problematic behaviour starts, Mr. Jocko acknowledges that there is also a dire need to support older demographics, too.
Chapter eight
Some of the strongest measures against drug traffickers and the ills they bring have come from a grassroots level, such as when First Nations in the Manitoulin Island and North Shore area have used their authority to safeguard their people.
Last year, Sagamok Anishnawbek created a checkpoint at its border to block non-essential traffic. The main purpose of this was to thwart the first wave of COVID-19 but the gimaa said a community member’s recent drug trafficking charge was an added reason for the restrictions.
M’Chigeeng set up three border checkpoints at the highway entrances to its territory last spring, a move that blocked highways across Manitoulin and angered many Islanders. Those checks were, too, in defense of COVID-19, but they also informed the community of who was entering their lands and for what purposes.
Road checks were a key part of concerned grandmothers’ actions against drugs in Wiikwemkoong in 2012, in response to community safety concerns.
In 2017, drug-related violence returned to Wiikwemkoong in the form of a violent assault. The grandmothers reunited and helped to co-ordinate a productive meeting with community officials and safety services.
The rate of mental illness and addictions has only grown since that time.
On February 22 of this year, Atikameksheng Anishnawbek, near Lively, declared a state of emergency over parallel mental health and addictions crises. More than 25 percent of recently deceased community members had a history of substance use disorder, and two-thirds had anxiety or depression.
Chief and council cited death statistics from 1992 to 2014, which showed Atikameksheng had a 1.5-times higher death rate than all of Ontario. Across North Shore First Nations, the average death rate was 30 percent higher than Ontario, according to a health provider.
Good Samaritan Act
The Good Samaritan Drug Overdose Act is part of the government’s comprehensive approach to addressing the crisis.
The Act can protect you from charges for:
- Possession of a controlled substance (i.e., drugs) under section 4(1) of the Controlled Drugs and Substances Act.
- Breach of conditions regarding simple possession of controlled substances in pre-trial release, probation orders conditional sentences and parole.
The Good Samaritan Drug Overdose Act applies to anyone seeking emergency support during an overdose, including the person experiencing an overdose.
The Act protects the person who seeks help, whether they stay or leave from the overdose scene before help arrives. The Act also protects anyone else who is at the scene when help arrives.
The Act does not provide legal protection against more serious offences, such as outstanding warrants, production and trafficking of controlled substances, all other crimes not outlined within the Act.
On March 25, M’Chigeeng declared its own social state of emergency over opioids, community safety, mental health and violence. Ogimaa-kwe Linda Debassige spoke directly with her community in a Facebook Live event to explain the declaration, and issued notices for further details. According to Ogimaa- kwe Debassige, 80 community members are currently living with opioid addiction. That’s 8.5 percent of M’Chigeeng’s onreserve population of 939, per 2018 figures.
In the first three months of 2021, she said, 35 percent of all paramedic calls for suspected overdoses in the District of Manitoulin happened in M’Chigeeng, which has just seven percent of the district’s population.
“Our existing programs and services for mental health and community safety are grossly underfunded and inadequate to meet the needs of the community. The staff are overwhelmed, the members of our community continue to feel unsafe, the elders are fearful and young people continue to be targeted,” she said in a community notice.
“We’ve had too many deaths in the community,” said Art Jacko, M’Chigeeng’s enaagdenjged (band manager). “Enough talk, it’s time for action and for everyone to work together to resolve this issue.”
M’Chigeeng appealed to the Canadian and Ontarian governments, OPP, RCMP and the Canadian Rangers, both for immediate assistance and for long-term support to manage the issue in the long-term.
Chief and council also reaffirmed M’Chigeeng’s commitment to being a drugfree community and vowed to remove drug dealers, including band members and those from away.
Its community protection bylaw allows the administration to block individuals from coming within a certain distance of another person or persons, and to evict people from community-owned housing if they pose a threat to the health and safety of the community.
M’Chigeeng has its own drug strategy group separate from Manitoulin Drug Strategy, has an opioid emergency operations group and has formed a mental health, addictions, community wellness, cultural and protection department to promote well-being and, hopefully, prevent people from starting to use drugs in the first place.
According to the Ogimaa-kwe’s notices, the federal government has indicated willingness to support M’Chigeeng’s shortterm needs, a pledge for which the community is grateful, but it has not committed to any long-term sustainable resources for the issue.
The notice did not state whether it had heard back from the provincial government. The Expositor has asked Ogimaa-kwe Debassige and Mr. Jacko for updates on government supports, but has not received any responses.
Aaron’s story
Aaron Case has found fishing to be an important tool in his healing process.
Aaron Case of Sheguiandah, a landbased counsellor at Gwekwaadziwin Miikan, an addictions treatment centre in Aundeck Omni Kaning, has dedicated himself to helping others recover from the same life he once lived, a life he almost lost through an overdose.
Mr. Case first used cannabis recreationally in high school and soon developed a dependence on the substance. When he went to college he moved to cocaine, then crack cocaine.
He began to use opioids recreationally and after a back injury, his prescription for Percocet wasn’t strong enough to dull the pain because he had built up so much tolerance.
“I’d take more and more and before I knew it, I was taking 20 to 25 tabs a day. That’s when the lying, cheating, stealing starts taking place because you can’t afford your habit,” he said.
Mr. Case moved west to work in the oil patch—a well-paid but gruelling sector whose workers often face substance use and mental health challenges, as seen in the rates of their employee assistance program usage. He says the lifestyle was firmly centred around working hard and partying harder.
“I was scrounging to even eat when I was at work; I was calling (my girlfriend) to help feed me while I was making $350 or $400 a day—it didn’t make sense,” he said.
He withdrew from his friends and family back home; at one point his partner did not even know if he was still alive. One of his friends got badly beaten by a biker gang and warned Mr. Case to leave town. He booked a ticket to Ontario and left with the clothes on his back.
“When I picked him up at the airport, he looked like Gollum (a Lord of the Rings character). I was shocked at the person I picked up at the airport,” said his partner, Alicia McCutcheon.
That scared Mr. Case into getting clean for about a year, but he was still using an opioid prescription for his back. At that time, doctors were beginning to reduce prescriptions as the dangers of opioids became clearer.
Mr. Case began to seek opioids in any way he could get them. He was back to his old usage habits. Despite the usage, he described himself as a “high-functioning” addict who maintained his commitments, and volunteered in the community. After 15 years of hiding his habit, he said he learned what he could get away with.
The relative stability ended abruptly when Mr. Case rolled his car and spent 11 days in critical condition in intensive care. “(Doctors) said the amount of painkillers they were giving him would have killed anyone else,” Ms. McCutcheon said. “That was just to dull his pain. It was absurd how high his tolerance was.”
Aaron Case says that despite the great strides he’s made in recovery, he still feels the sting of stigma.
“(Doctors) said the amount of painkillers they were giving him would have killed anyone else,” Ms. McCutcheon said. “That was just to dull his pain. It was absurd how high his tolerance was.”
He received slow release fentanyl patches, hydromorphone and Dilaudid pills when needed, all kept under the watch of his partner, but Mr. Case’s addict brain took over. He was soon using a week’s supply in mere days and his breathing would slow to a near overdose state.
To this day, Ms. McCutcheon has audio recordings on her phone of his laboured breathing and the characteristic “death rattle” of a fentanyl user close to overdose.
Doctors eventually cut him off, but his addiction problem was still active. Mr. Case had begun seeing Dr. Lionel Marks de Chabris for opioid withdrawal support but he was still using illegal supplies like heroin.
It almost killed him. “It was a Wednesday. Aaron had to be at his appointment (with Dr. Lionel) and I kept calling him to remind him to be on his way, and I just got this overwhelmingly horrible feeling,” Ms. McCutcheon says.
For the first (and last) time, she decided to track his phone and it placed him at a Little Current apartment. She drove over and saw two unfamiliar men gesturing wildly from inside the apartment. They soon ran to their car and sped away.
The door was locked so she called the tenant’s mother as well as a lifelong family friend. Both arrived around the same time and they found Mr. Case lying on his back, blue in the face.
He wasn’t breathing. The others screamed at Ms. McCutcheon to get away and she raced to her parents’ home to grab a naloxone kit she had picked up that summer during the Pride Manitoulin celebrations, all while calling 9-1-1. It wasn’t enough to reverse the overdose. The family friend performed CPR.
The paramedics arrived and put him on oxygen to stabilize him after he began to come to. However, they were not particularly sympathetic.
“The paramedic was a complete f***ing asshole. He was treating me like a piece of shit and one of the responding cops made a nasty comment, like ‘he made it this time, but we’ll see about the next time’,” Mr. Case said.
Ms. McCutcheon turned to one of the attending officers and said “‘mark my words, this is just the start (of the opioid epidemic).’ And it was. This was five years ago.
After Mr. Case was resuscitated, the couple drove to Espanola for his Dr. Lionel appointment.
They made it on time.
Aaron Case knows the great joy that sobriety can bring and hopes to bring that joy to others through his position as a land-based addictions counsellor.
“That was a wake-up call. I was still using, at minimum amounts just to function through the day and not be sick, but I was still an addict. Then, there was an ultimatum from Alicia. Either I go get help, or I’ve got to go,” Mr. Case said.
Mr. Case entered care at Toronto’s Bellwood Health Services, a nation-leading rehabilitation centre that offered a six-week program plus aftercare, which is much more effective than government-funded programs that only last for a month.
Mr. Case reconnected with old friends and embraced a healthier lifestyle after his return. Then, Gwekwaadziwin Miikan gave him a chance at employment.
He’s been able to use those lived experiences to empathize with the people he helps to treat through Gwek’s land-based healing programs.
“If you don’t know what they’re actually feeling, how are you supposed to understand what they’re going through?” he said of the people he now helps.
Mr. Case tried attending Narcotics Anonymous for nine months but meetings often left him feeling worse, so he found other outlets for recovery. He credits his friend Dave Patterson for reminding him of his love of fishing and Mr. Case is now a key member of the ‘Ontario Fishing Guys’ and a pro-staffer for a number of fishing-related businesses.
Two years before his near-fatal overdose, Mr. Case began seeing Dr. Lionel for his addiction. The two remain close.
“If not for him and Alicia, I’d probably be dead. He worked with me through those three or four years, where I was a full-fledged addict all the way through,” Mr. Case said.
The stigmatization he faced while accessing treatment was disheartening. He has had three family doctors over eight years and he faced consternation from pharmacists and the public when he picked up his suboxone doses.
“Alcoholics don’t really get judged as much but drug addicts are in a different lens. If you’re a heroin or a pill user, you’re a piece of shit in their eyes. But everybody’s the same, you can’t control what you’re doing, so why is somebody better than me?” Mr. Case said.
He has now gained the tools he needs to avoid repeating his past struggles and his brain has returned to being able to process right from wrong, a function that substance use disorder impairs as drugs take priority over everything else in a user’s life.
“I thought I was so broken that I was going to be broken for life. I really did,” he said.
While many people have celebrated Mr. Case’s story of redemption, Ms. McCutcheon said she often felt left behind after living through several years of hell while trying to bring back the man she once knew.
“I was living for two people. I’ll admit I was frustrated when he came back from treatment and all the heroism that came with it, I felt resentful,” she admitted. “I was so happy for him, of course, but I felt as though I had run a marathon with him on my back, but he got all the credit.”
“We lived together and never stopped loving one another, but we were like two ships passing in the night,” she said. “He was just this shell of a person who put one foot in front of the other, but I was there making sure he was not doing anything stupid, and doling out money to pay for things to make sure he didn’t get any worse. It was horrible.”
That drove her toward unhealthy coping mechanisms, too. “I drank too much, for sure, on the weekends during the throes of (Mr. Case’s) addiction. It was my escape from reality for a bit, to have a few drinks and pretend everything was fine,” Ms. McCutcheon said.
Her immune system was in overdrive and she never fell ill during the worst of Mr. Case’s addiction, but she has faced a steady raft of illnesses since his recovery.
“Things started to fail me a bit. I realized, too, that I needed some help. I had anger issues; I lived in a constant state of dread and worry, and in sadness at the way Aaron had been treated during his illness. I really couldn’t find, although I tried, any support for myself that I thought would address my issues. I ultimately stopped feeling the way I was feeling on my own,” she said.
Ms. McCutcheon turned to journalism, both as an outlet for her discontent with the lack of services available on Manitoulin and to help raise awareness of the issue. That effort, she said, hopefully offered support to others who may be living through a similar ordeal. It has also ensured these issues remain part of public discourse, to hopefully support work toward solutions.
The couple is happy, and healthy, in Sheguiandah.
Chapter nine
Many Islanders are at a crossroads as they either deal directly, or indirectly, with opioid crisis.
Arriving at longer-term solutions to the opioid and overdose crises may require difficult conversations about why people begin to experience addictions in the first place.
In the view of Dr. Menzies, the most common root cause of addictions is trauma. “You can’t just take a pill and be better.
When you break down anxiety and depression, a lot of it was developed when they were kids,” says Dr. Menzies, adding that he believes therapy is a better long-term solution.
Not every case of addiction stems from trauma but professionals who support people with substance use disorder say it is a very common factor in addictions and mental illness.
“When I see people, I don’t criticize them for drinking or doing drugs. To me, I recognize it’s a sense of relief. It gives them pleasure and helps them to forget things. My role is to give them something else they can substitute with that,” says Dr. Menzies.
He says many of his patients, especially younger ones, struggle with belief in themselves. Trauma can also interfere with a child’s learning ability, which can lead to higher drop-out rates and lower one’s potential for advancing in life.
Trauma not only impacts the person who holds it; it also affects every person who interacts with that individual. This is the foundation for intergenerational trauma, when one generation unwittingly passes their traumas down to their children, who may inherit some of the same behaviour, creating a cycle.
Intergenerational trauma appears in people of all backgrounds, says Dr. Menzies, but Indigenous peoples in Canada have disproportionate rates of the condition due to decades of harmful Canadian policies that actively sought to strip Indigenous children of their cultural identity and remove them from their families during their developmental years.
Dr. Menzies says the impacts of residential schools often appear in attachment and abandonment issues, as well as negative selfimage. When the students came home, they carried all of the mental and emotional impacts from those schools.
These became highly visible when the former students began to start families. Many lacked parenting skills and the ability to bond with their children, says Dr. Menzies, which meant children’s aid societies intervened, especially during the Sixties Scoop. because many parents could not care for their children.
“There’s that cycle, so kids wind up in care and again you get more abandonment issues of ‘how come my parents don’t love me, why am I living in a stranger’s home?’” Dr. Menzies says.
He speaks from experience.
“I grew up institutionalized in Children’s Aid. I had no emotional care for me, I was abandoned, I had attachment issues and I went through a lot of trauma,” he says.
After he aged out of care, he was homeless and began to use drugs and alcohol.
“When we were growing up, a lot of us thought we wouldn’t be around until age 20,” Dr. Menzies says. “Here I am with my PhD, and hopefully the work I’m doing is helping to change lives.”
When I see people, I don’t criticize them for drinking or doing drugs. To me, I recognize it’s a sense of relief. It gives them pleasure and helps them to forget things. My role is to give them something else they can substitute with that.
Processing one’s past is a crucial step in ending addictions, Dr. Menzies says, or else the patient will likely turn to other vices and can develop anger over their seeming lack of progress.
Professional help can ease the healing process but the individual has to commit to regular self-reflection and finding creative outlets or healing processes to release their energy and deal with their past.
In First Nations in particular, where intergenerational trauma is so widespread, entire communities may have to do such work.
“Within traditional aboriginal culture, the community’s support is critical for the development of individuals and families. Holistic healing is not achievable without the influence and guidance of a balanced and healthy community,” Dr. Menzies states in a 2010 article in Native Social Work Journal.
It will be a monumental undertaking.
“If we, together, as a community, put as much effort together that we did over the past year with COVID- 19, and we focus that same effort into dealing with addictions, maybe we’ll make a difference,” says Roger Beaudin, manager of M’Chigeeng Health Services.
Another community-wide trauma source present on Manitoulin is from three priests who abused children in Wiikwemkoong in the mid-20th century. Dr. Menzies has worked with the victims of Father Epoch (the principal abuser) in other First Nations and says many people have turned to substances to cope. Several have boundary issues or have repressed their experiences, among other challenges.
But Jesuits have also brought plenty of good things to Wiikwemkoong over past centuries, including supporting chiefs in their decisions not to sign treaties and to remain unceded. The church holds much respect and many community members still refuse to discuss the issue, according to some survivors.
“Keeping secrets within communities divides the community. It pits families against families and … people leave communities because they can’t deal with the secrets,” Dr. Menzies says.
But any healing initiatives have to be thoughtful and rooted in care. Having a guest speaker in for one day and not offering followup supports may inadvertently cause more harm, he says.
Gwekwaadziwin Miikan land-based counsellor Eddie Gough says he understands the power of community-based healing because reconnecting with his culture helped to save his life.
“Especially with addictions, the opioid epidemic, that’s not a thing a single person can heal from. It takes the whole community, not just the people struggling with addictions or the people providing social services,” Mr. Gough says. “One person can’t heal if the rest of the community is hurting them.”
He says once individuals heal, they will be able to help even more people through partnerships with social services, elders, youth, police and the justice system.
Conclusion
Manitoulin is home to many lighthouses, casting a beacon of light and a way home for mariners, just as the many people and organizations who are on the front lines of the opioid crisis aim to do.
Finding and delivering effective solutions to the opioid crisis on Manitoulin Island will be a massive undertaking, but there are promising developments across the region that may help with this burden.
Despite its impacts that have deeply worsened the opioid crisis across Canada, the COVID-19 pandemic has had at least one benefit: community leaders across Manitoulin Island are working together more than ever before, including through bi-weekly meetings of the Manitoulin COVID-19 Leadership Co-ordination Committee.
At those meetings, the leaders talk about the issues common to all Islanders, such as the opioid and mental health crises, and explore ways they can work together to get more support for these ills.
Manitoulin may have the highest amount of local political capital it’s ever had to address this crisis, but Mayor MacNevin says better information sharing is still required to make the changes more meaningful.
There are also more recovery programs in the area such as Northwood Recovery and Ngwaagan- Gamig (Rainbow Lodge), many of which have innovated new, effective ways of treating substance use disorder and mental illness. Gwekwaadziwin Miikan, a new entrant to this field, offers 90-day land-based treatment with live-in aftercare and community supports after that period to ensure its clients gain long-term benefits.
Innovative programs, most common in First Nations, to help young people avoid the cycles of mental illness and addiction, are showing promising results. More access to these programs in all communities could reduce the future costs of treating such ailments and save lives in the process.
If Manitoulin is to address the opioid and mental health crises in an effective way, it will require more than the innovation of leadership. Every person across the Island must recognize and fulfill their role in creating healthy, supportive communities.
“I think the public can educate themselves on the dangers of opioids, understand that addiction is a medical condition that affects all walks of life, and be caring, compassionate and understanding,” says Mr. Gauthier, the pharmacist.
Every citizen can help immediately by choosing compassion for their fellow citizens who are trying to break free from substance use. They can also make direct impacts by carrying a naloxone kit to possibly save someone’s life if they overdose, as well as reporting criminal activity to police or Crime Stoppers.
“People see things differently, which means you have some details that others may not, and it is often all the little details put together that help officers make the case,” states a UCCM Police appeal for information. “Community members serve as the eyes and ears of the community.”
A harm-reduction mindset includes immediately calling emergency services for a suspected overdose, even if the drugs are from an illegal supply.
The federal Good Samaritan Drug Overdose Act, 2017, means people who call emergency services for someone who is overdosing cannot be charged for illegal drug possession.
Innovative solutions from any source will go a long way toward healing Manitoulin.
The statistics tell a chilling story. Paramedics have responded to more than 80 suspected overdoses in the past three years on Manitoulin Island alone and more than 15 people have died directly from opioids since 2015.
Every one of those numbers represents a lost human life, a hurt family and an unnecessary tragedy.
“This is our community; these are our people. Every person that dies is one of us,” says Ms. Groves, the Children’s Aid Society executive director.
A saying from the 1600s is that in tough times, the metaphorical ‘darkest part of the night’ comes just before the break of dawn.
May this be Manitoulin’s darkest hour.